The Harm vs. Good of Immediate Implant Placement
- Andre Chen

- Aug 17, 2025
- 3 min read
Sometimes in dentistry, I honestly don’t know if I’m doing better—or worse—for the patient. A small decision can feel enormous: an 8 year old kid with 5 Lower central invisors, which tooth should I take out? A wisdom tooth with high probability of infection, but dangerously close to the inferior alveolar nerve should I go in ? These are daily choices, and there isn’t always literature or evidence to guide you. It’s sometimes that and your experience, your gut feeling… and sometimes just a little bit of bravery. (I’m sorry the hater that going to say that it’s just science but in real life practice , this is also important)
I recently received a crazy case: external root resorption on #21 and #11. The patient, a 40-year-old woman with a high smile line, came to me saying, “Dr. Chen, after going to universities and several doctors, they referred me to you!” That feeling of trust was amazing… but it lasted only five minutes. I did the CBCT and… bang. Internal and external resorption like I had never seen before.
How do you tell a 40-year-old woman that she’s going to lose her two front teeth? That’s a bad day for the dentist—and an even worse day for the patient.
She had already seen several colleagues, and everyone essentially passed her on. When I looked at the CBCT, the most difficult decision I had to make was whether to place implants immediately, or extract and preserve the sockets for delayed placement—or extract, wait six weeks, and do early implant placement with GBR, as described by Stephen Chen (Chen, 2008).
Thinking It Through
First, I go back to ITI Volume 1 principles:
Smile line: This patient’s was very high, which makes the case immediately more challenging.
Papilla and interproximal tissue: You need to ensure papilla stability, or black triangles will compromise the result. In this case, the lateral incisors’ mesial attachment was preserved, which was a plus. The papilla between the centrals was still intact, so even minor interproximal attachment loss could be managed aesthetically.
Buccal plate: All or nothing. Partial loss? Delayed implant placement (Morton et al., 2018) Full loss?
Here, the buccal plate was intact—favorable for immediate placement.
Apical bone for stability: Enough native bone? Primary stability guaranteed.
All the factors aligned for immediate implant placement. Waiting six months would have required a temporary solution, like a removable or Maryland bridge, which simply would not have met her esthetic needs.
Implant Choice
For immediate placement, I go for a very aggressive thread design. Why? It engages the bone immediately for primary stability. A non-aggressive conical implant sometimes relies too much on bone compression, which can be more traumatic than a self-tapping thread.
Drilling: The Jedi Way
Precision over speed, always.
Position the patient with chin up, central incisors at 45° to the floor.
Spear drill to map the palatal wall, trusting your eyes and feel.
Step gradually through drills (2.2 → 2.8 → 3.5 mm), adjusting angles to respect palatal anatomy.
Go cautious. Feel the cortical resistance, then the softer trabecular bone. Trust your gut, Luke. Let it go.
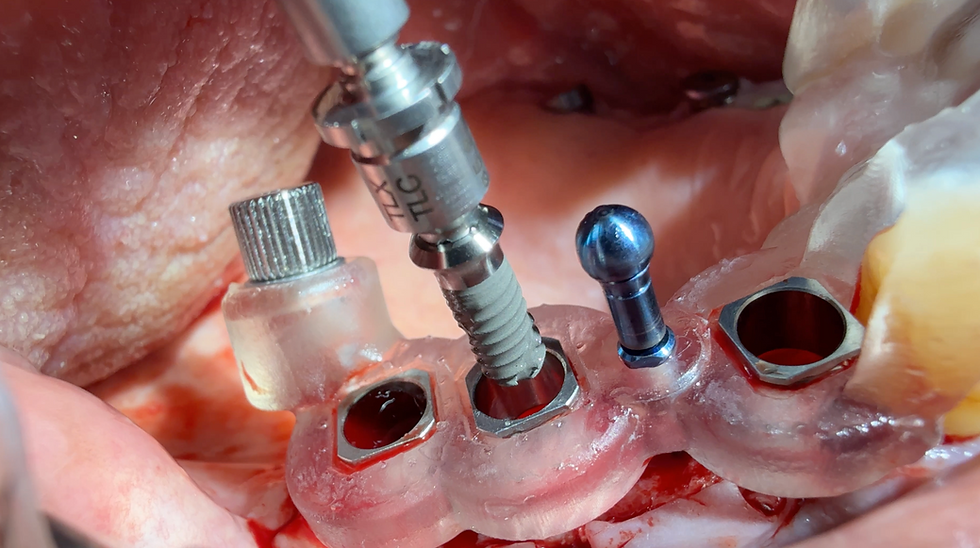
Implant Placement
Aggressive threads engage quickly. Just a few turns, careful hand ratchet adjustments, and keep a sharp eye on the buccal side to avoid displacement.
Provisional Restoration
Before grafting, adapt the provisional to capture the emergence profile. CAD/CAM PMMA provisionals help avoid excessive acrylic in the tissues.
Grafting and Soft Tissue
Xenograft: Compact into the jumping gap gently, suctioning excess saline.
Soft tissue graft: Subepithelial connective tissue grafts can enhance the profile. In this case, we did one at #11.
Occlusion and Final Checks
Remove all contacts in centric and eccentric occlusion.
Radiograph to confirm everything is tight.
Following these protocols, tissue response is predictable, and patient acceptance is high. Sometimes I wonder if I’m doing the right thing—but in cases like this, with careful evaluation, planning, and execution, I clearly feel that immediate implant placement was the right choice.
Tough case. Definitely one for the books.
References:
ITI Treatment Guide Volume 1: Implant Therapy in the Esthetic Zone – Single-Tooth Replacements. ITI Academy
Chen, S. (2008). Immediate or Early Placement of Implants Following Tooth Extraction: Review of Biologic Basis, Clinical Procedures, and Outcomes. ResearchGate PDF
Morton, D., et al. (2018). Risk Assessment for Immediate Implant Treatment. Decisions in Dentistry



Comments