The Art of Hidden Information in 2D Radiographs
- Andre Chen

- Sep 18, 2025
- 3 min read
I’m fascinated by how imaging has evolved in the latest years! The innovations are extraordinary, and also the low radiation for 3D images allows not only to irradiate only the anatomical part we are working on, but due to its low radiation we can use it to control the position of the implants.
In the past we finished the surgery and did a periapical radiograph or a panoramic X-ray! But the question nowadays is :
why do we do it ? and what’s the clinical information that we can take to the clinical arena.?

“The eye sees only what the mind is prepared to comprehend.” — Henri Bergson
When we look at the world, we like to believe our eyes give us an objective picture of reality. But perception is never neutral — it is filtered by our experiences, our knowledge, and even our biases. Often, we see things that are not there, or fail to notice what is right in front of us.
So on 2D we sometimes see implants biting and hitting neighboring teeth that are not there (the spatial compression), or sometimes implants that seem ok but in reality are in poor or wrong bone positions, affecting the outcome of the case.
But, if our education and clinical expertise are sharp (and that only come with clinical expertise), you immediately understand that to truly evaluate an implant either you take a localized CBCT or you use a scanbody with an intraoral scanner and put it in “treatment evaluation – coDiagnostiX,” and voilà, you get to know everything about implant position.
To illustrate a common everyday clinical challenge, yesterday I treated two cases that demonstrate how technology can guide us toward proper implant placement
Case 1: The Premolar
The pure one-piece in the traditional premolar site — in this case, we placed an implant on number 24 — and you can see the different information in 3D.
If I had taken a panoramic or periapical X-ray, the chances of superimposition would have been misleading, and I might have had second thoughts, possibly retrieving the implant to place it with the tip distally.
Is it wrong? Not necessarily. But in that case, you are doing a “radiographic-driven surgery,” and the chances that you lose primary stability are huge, just because you are drilling a second site. The area now has the extraction hole, the initial hole, and now a second hole in a closed-flap post-extraction scenario...... That may be too hard to handle… and eventually you end up with no implant, no crown and no immediacy… in an esthetic area with high-expectation patients… good luck 🍀.
Case 2: Two Adjacent Narrow Implants
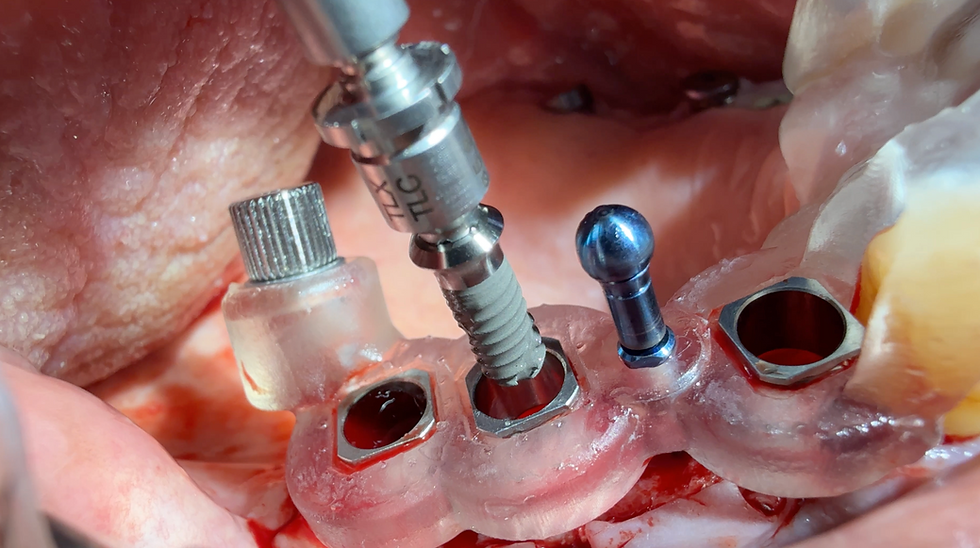
Or the second case, about 2 adjacent implants, 3.3 Starumann BLT, very narrow.
Here I was almost perforating the buccal bone in the anterior one (#14). The problem here is even harder: you have #14 and #15 to place in a tiny area for premolars, but the root of #13 is tilted distally, and the root of #16 is tilted mesially 🤔.
Another problem is that, although the area of #14 is a residual crest, #15 is a residual root that is rotated, meaning that the hole left by the extraction leaves a mesiodistal defect that makes parallelism and implant placement harder.
So first: I drilled #14 parallel to the tooth of the canine and placed a pin, and then I drilled #15 parallel to the root of #15 and placed a pin.
Then I made a localized CBCT, and if I had taken only a normal periapical, chances are that everything would have come superimposed, and I would not have gotten any reliable information. Or maybe it would have looked ok in relation to the adjacent teeth — but I would never have spotted that the implant was tilted to the buccal area, almost perforating the buccal bone. More critically, I didn’t engage the palatal bone, therefore compromising stability, the healing phase, and eventually the survival of it.
You cannot have this information on a 2D radiograph; the sagittal information is crucial and vital for your performance
Now the CBCT just gave me my reference! Drill to the palatal of the initial drilling and you are into the palatal side! And voilà — 2 implants in the prosthetically correct position given by the arch and adjacent teeth, engaging native bone, with apical tapered macrogeometry so they don’t meet at the apex, 1.5 mm apart from adjacent teeth and 3 mm apart from each other for correct biological width formation!
The Takeaway
That’s technology at your service without sacrificing patient radiation, thanks to the low-radiation protocols.
Be smart and sharp — autumn’s solstice is arriving!!!!



Comments