Subcrestal, Supracrestal, and One-Piece Implant Placement in the Posterior Mandible
- Andre Chen

- 16 hours ago
- 5 min read
A Prosthetically Driven Concept and the Importance of Three-Dimensional Accuracy
The Dream of the Supracrestal Implant
Four approaches. Four levels of precision.
This morning I woke up with one of those thoughts that doesn’t come from reading a paper…
It comes from living implant dentistry.
I slept well.Body Battery: 100%.Sleep Score: 95%.
And maybe because of that…
I dreamed about implants.
Not an abstract dream.A surgical dream.A prosthetic dream.
And the message was simple, but powerful:
The more supracrestal an implant is, the more perfect its three-dimensional positioning must be.
Suddenly, everything became clear.
Posterior Mandible: Where Details Rule
Implant rehabilitation of posterior mandibular molars remains a frequent clinical challenge due to ridge morphology, limited soft tissue volume, and high functional loading demands.
Multiple surgical and restorative strategies may be applied, including:
subcrestal positioning
supracrestal platform concepts
wide-diameter implants
one-piece implant designs
A fundamental principle is that as the implant–prosthetic interface is positioned more coronally, the requirement for precise three-dimensional implant placement increases significantly, particularly in the bucco-lingual dimension.
This concept is consistent with ITI-oriented recommendations emphasizing prosthetically driven planning as a prerequisite for long-term biological and restorative stability.¹–³
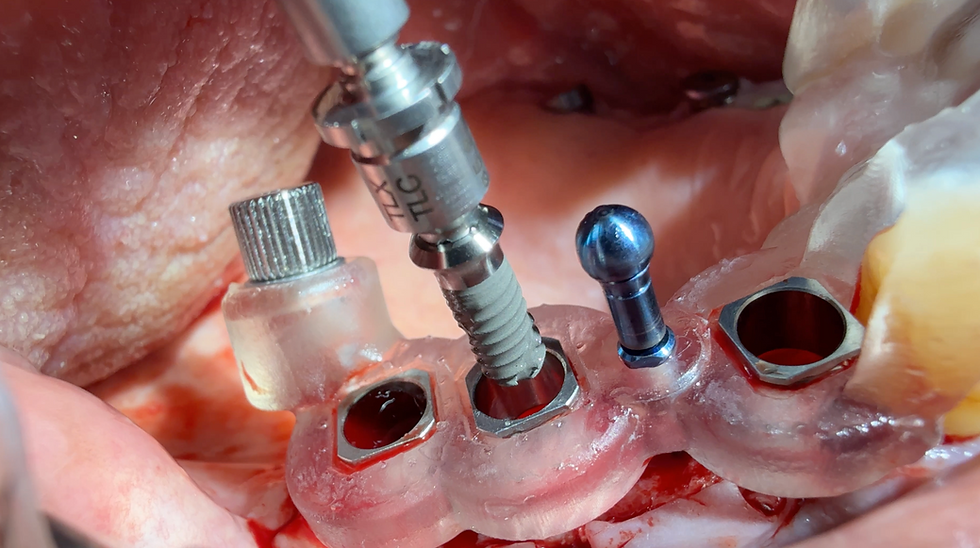
Four Clinical Situations
1. Subcrestal Implant Placement
Subcrestal positioning places the implant platform below the crestal bone level and often provides greater restorative flexibility.
In such cases, prosthetic correction may be achieved through:
intermediate abutments
angled abutments
cemented or screw-retained compensatory solutions
This approach offers a wider margin of correction regarding implant angulation and emergence profile management.³,⁴
2. Supracrestal Placement with Regular-Diameter Platforms
Supracrestal implant concepts, where the restorative platform is positioned approximately 2–3 mm above the crestal bone, may contribute to soft tissue shaping and emergence profile optimization.
In selected posterior cases, this strategy may reduce the need for extensive regenerative procedures.
However, supracrestal placement requires increased accuracy in:
apico-coronal positioning
mesio-distal spacing
bucco-lingual orientation
Because the restorative interface is located within the soft tissue zone, positional deviations may directly influence tissue stability and patient comfort.²,⁵,⁶
3. Supracrestal Placement with Wide-Diameter Platforms
Wide-diameter implants (5.0–6.0 mm) are frequently indicated in molar sites to improve emergence profile and load distribution.⁷
Nevertheless, supracrestal positioning combined with increased platform diameter substantially reduces tolerance for bucco-lingual errors:
Lingual over-positioning may result in tongue interference and patient discomfort
Buccal over-positioning may increase the risk of soft tissue recession due to keratinized mucosa displacement
Thus, wide-platform supracrestal implants require strict prosthetically driven planning and controlled surgical execution.⁶–⁸
4. One-Piece Implant Systems and Ceramic Implantology
One-piece implant designs, frequently applied in ceramic implantology, present the highest demand for surgical precision due to the absence of prosthetic correction options.
Since the abutment is integrated into the implant body, restorative flexibility is minimal, making three-dimensional placement critical from the initial osteotomy.
This is particularly relevant in zirconia implant systems, where one-piece configurations remain common and require exact positioning to ensure long-term functional and biological success.⁹
Clinical Implications
All four approaches represent valid treatment modalities when appropriately indicated.
However, a progressive increase in positional demand can be observed:
Subcrestal placement provides restorative flexibility
Supracrestal placement increases soft tissue influence and reduces correction potential
Wide platforms amplify bucco-lingual sensitivity
One-piece implants require absolute surgical accuracy
Consensus-Oriented Conclusion
As the implant–prosthetic interface moves coronally and prosthetic correction options decrease, the requirement for precise three-dimensional implant positioning becomes critical.
In posterior mandibular rehabilitation—particularly with supracrestal and wide-platform concepts—prosthetically driven planning and controlled surgical execution are essential to ensure long-term tissue stability, patient comfort, and restorative success.¹–³
The Conclusion of the Dream
All four approaches are valid.
But there is an invisible rule:
The closer we move toward a one-piece concept, the more absolute the planning must become.
Subcrestal implants forgive.Supracrestal implants demand.Wide platforms punish mistakes. One-piece implants accept none.
And in the end…
This is implant dentistry.
Not placing screws. But positioning future tissues.
Surgery is freedom… until prosthetics can no longer save us. And on that day, the implant must already be exactly where it should have been from the very first drill.
Clinical Recommendation (Take Home message )
Clinical Recommendations: Supracrestal Implant Placement in the Posterior Mandible
• Prosthetically driven planning is essential when supracrestal implant concepts are applied in posterior mandibular molar sites, as the restorative interface is positioned within the soft tissue zone.¹–³
• Three-dimensional implant positioning must be strictly controlled, with particular emphasis on the bucco-lingual dimension, since minor deviations may directly affect patient comfort, emergence profile, and soft tissue stability.²,⁶
• Subcrestal implant placement provides greater restorative flexibility, as prosthetic components (e.g., intermediate or angled abutments) may compensate for moderate positional discrepancies.³,⁴
• Wide-diameter supracrestal platforms require increased surgical accuracy, as buccal over-positioning may increase recession risk, while lingual displacement may result in tongue interference.⁶–⁸
• One-piece implant systems, particularly in ceramic implantology, demand the highest level of precision, as prosthetic correction options are minimal or absent and implant positioning must be exact from the initial osteotomy.⁹
• Clinical decision-making should consider soft tissue phenotype, ridge anatomy, platform diameter, and prosthetic correction potential, recognizing that coronally positioned interfaces reduce tolerance for error.¹–³
Consensus Summary
As the implant–prosthetic interface moves coronally and prosthetic correction options decrease, precise three-dimensional implant placement becomes critical to ensure long-term tissue stability, patient comfort, and restorative success.
References
Buser D, Martin W, Belser UC. Optimizing esthetics for implant restorations in the anterior maxilla: anatomic and surgical considerations. Int J Oral Maxillofac Implants. 2004;19(Suppl):43–61.
Gallucci GO, Benic GI, Eckert SE, Papaspyridakos P, Schimmel M, Schrott A, et al. Consensus statements and clinical recommendations for implant loading protocols. Int J Oral Maxillofac Implants. 2014;29(Suppl):287–290.
Hämmerle CHF, Chen ST, Wilson TG Jr. Consensus statements and recommended clinical procedures regarding the placement of implants in extraction sockets. Int J Oral Maxillofac Implants. 2004;19(Suppl):26–28.
Cochran DL, Buser D, Ten Bruggenkate CM, Weingart D, Taylor TM, Bernard JP, et al. The use of reduced healing times on ITI implants with a sandblasted and acid-etched surface. Clin Oral Implants Res. 2002;13(2):144–153.
Grunder U. Stability of the mucosal topography around single-tooth implants and adjacent teeth: 1-year results. Int J Periodontics Restorative Dent. 2000;20(1):11–17.
Buser D, Chappuis V, Belser UC, Chen S. Implant placement post extraction in esthetic single tooth sites: when immediate, when early, when late? Periodontol 2000. 2017;73(1):84–102.
Renouard F, Nisand D. Impact of implant length and diameter on survival rates. Clin Oral Implants Res.2006;17(Suppl 2):35–51.
Spray JR, Black CG, Morris HF, Ochi S. The influence of bone thickness on facial marginal bone response: stage 1 placement through stage 2 uncovering. Ann Periodontol. 2000;5(1):119–128.
Cionca N, Hashim D, Mombelli A. Zirconia dental implants: where are we now, and where are we heading? Periodontol 2000. 2017;73(1):241–258.



Comments